The Robot Surgeon Will See You Now: How AI and Automation Are Revolutionizing Stroke Care from 4,000 Miles Away
A New Dawn for Medicine: Surgery Across an Ocean
Imagine this: a patient in a rural hospital suffers a major stroke. The nearest specialist capable of performing the life-saving surgery is hundreds, if not thousands, of miles away. The clock is ticking—every minute that passes, millions of brain cells are lost. Traditionally, this story often ends in tragedy or lifelong disability. But what if the world’s best surgeon could be in that operating room in minutes, their hands guided by a robot, their eyes seeing through a high-definition camera, all from the other side of the planet?
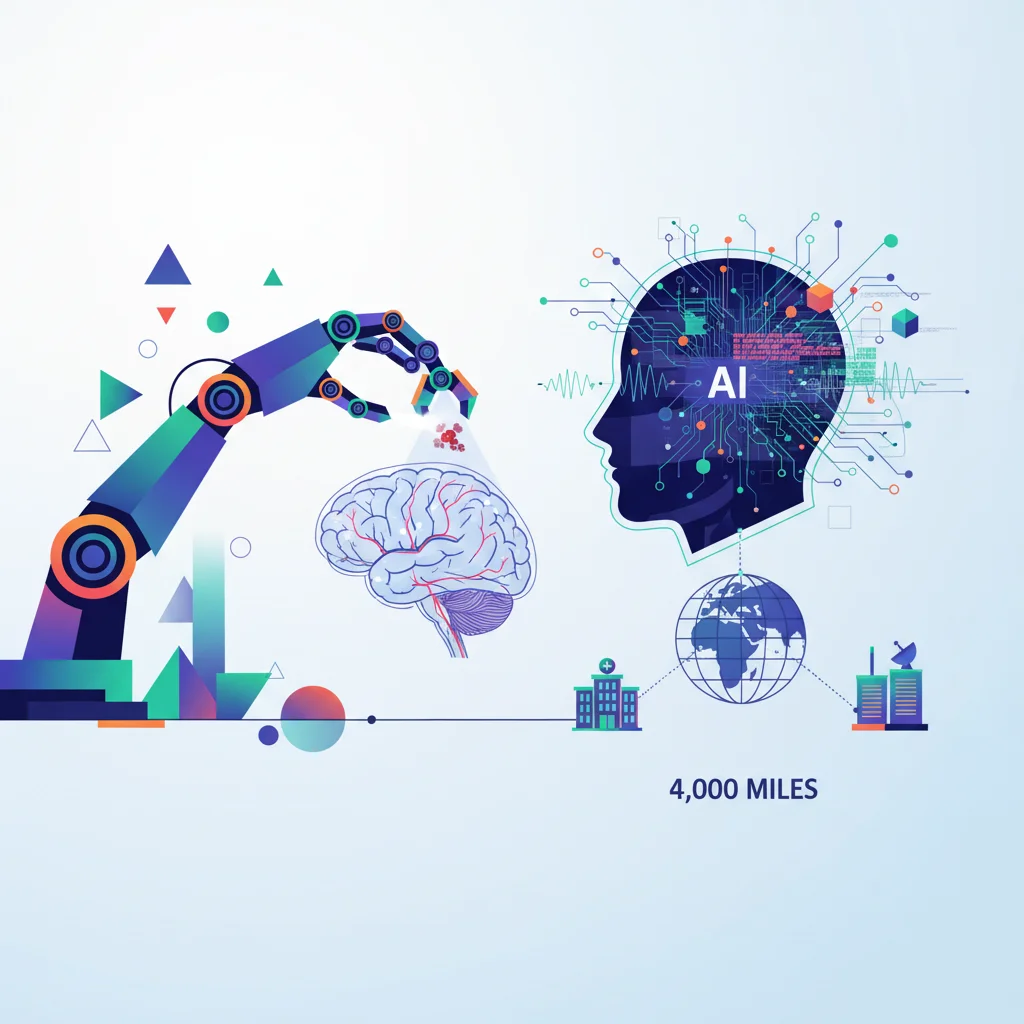
This isn’t a scene from a sci-fi movie. It’s the groundbreaking reality demonstrated by a team of surgeons in Dundee, Scotland, and the United States. In a world-first, a professor successfully performed a remote thrombectomy—a delicate procedure to remove a blood clot from the brain—on a realistic human cadaver. The surgeon was in Dundee, while the “patient” and the robotic system were in Boston, nearly 4,000 miles away. As reported by the BBC, this landmark achievement isn’t just a medical marvel; it’s a profound statement about the future of healthcare, a future powered by innovation, sophisticated software, and global connectivity.
For developers, tech professionals, and entrepreneurs, this breakthrough is a clear signal. The operating room is becoming the next frontier for high-stakes automation, artificial intelligence, and cloud-based platforms. This isn’t just about building a better robot; it’s about creating the entire ecosystem—from the SaaS platform that manages the procedure to the cybersecurity protocols that protect it—that will redefine emergency medical care.
The Stroke Problem: A Race Against Time and Distance
To grasp the significance of this achievement, we must first understand the enemy: ischemic stroke. This occurs when a blood vessel supplying blood to the brain is obstructed by a clot. It’s a devastatingly common and time-sensitive medical emergency. Globally, 1 in 4 adults over the age of 25 will have a stroke in their lifetime, and it is a leading cause of death and disability, according to the World Stroke Organization.
For many ischemic strokes, the gold-standard treatment is a mechanical thrombectomy. A neurosurgeon guides a thin catheter through an artery, usually from the groin, all the way up to the brain to physically retrieve the clot. The procedure is incredibly effective, but it has one major bottleneck: you need a highly trained specialist and a hospital with a specialized neuroradiology suite. These resources are concentrated in major urban centers, leaving vast rural and underserved populations at a massive disadvantage. This is often called the “tyranny of distance.” This remote robotic surgery aims to shatter that tyranny.
The AI Revolution in the Call Center: Annihilation or Evolution?
Deconstructing the Tech: More Than Just a Joystick
Calling this a “remote-controlled robot” is a vast oversimplification. This success is the culmination of decades of progress in multiple tech sectors. It’s a symphony of hardware, software, networking, and, increasingly, artificial intelligence.
The Software and Automation Core
At the heart of the system is a complex software stack responsible for translating the surgeon’s hand movements into the robot’s micro-movements with near-zero latency. The programming behind this involves advanced algorithms for motion scaling (allowing a large hand movement to become a tiny, precise robotic one), tremor filtration to eliminate natural human hand shakiness, and force-feedback simulation. This is high-stakes automation, where a single bug in the code could have catastrophic consequences. The goal is to create a seamless extension of the surgeon’s own senses and skills across any distance.
The Emerging Role of AI and Machine Learning
While the Dundee experiment focused on direct remote control, the next frontier is integrating AI and machine learning. AI algorithms are already being used to analyze brain scans faster and more accurately than the human eye, helping to identify the exact location and size of a clot. In the near future, we can expect to see AI co-pilots that:
- Provide real-time guidance to the surgeon by highlighting optimal pathways through arteries.
- Automate repetitive sub-tasks of the procedure.
- Use predictive analytics based on data from thousands of previous surgeries to warn the surgeon of potential complications before they arise.
This is where startups in the HealthTech space have a massive opportunity—building the AI-driven intelligence layer that makes robotic systems not just remote, but smarter.
Cloud, SaaS, and Cybersecurity Implications
How do you securely connect a surgeon in Scotland to a patient in Boston? The answer lies in the cloud. A robust, high-bandwidth, and ultra-low-latency network is the non-negotiable backbone of telerobotics. This infrastructure enables what could be considered “Surgery-as-a-Service” (SaaS), where hospitals don’t just buy a robot; they subscribe to a global network of available specialists.
However, this connectivity opens up terrifying new vectors for attack. The cybersecurity challenge is immense. A compromised surgical robot is the stuff of nightmares. Securing these systems will require a multi-layered approach, including end-to-end encryption, multi-factor authentication for surgeons, and constant network monitoring for intrusion detection. The integrity of the data and the control link is paramount. As a leading medical technology journal points out, ensuring the security of these devices is a “critical, life-or-death” challenge that requires a new level of collaboration between medical device manufacturers and cybersecurity experts (source).
To better understand the leap forward this technology represents, let’s compare the traditional approach with the new remote robotic paradigm.
| Feature | Traditional Thrombectomy | Remote Robotic Thrombectomy |
|---|---|---|
| Specialist Requirement | Specialist must be physically present at the patient’s bedside. | Specialist can be located anywhere in the world with a network connection. |
| Geographic Accessibility | Limited to major hospitals in urban centers. | Potentially available at any hospital equipped with the robot, regardless of location. |
| Time to Treatment | Dependent on patient transport time to a specialized center, often hours. | Can begin almost immediately upon diagnosis at a local hospital. |
| Key Technology | Fluoroscopy (X-ray imaging), catheters, guidewires. | Robotics, high-speed networking, advanced software, AI-assisted imaging. |
| Primary Challenge | Logistics and the “golden hour” time limit. | Network latency, cybersecurity, cost, and regulatory approval. |
The Human Impact: Democratizing Elite Medical Care
The ultimate promise of this innovation is not just technological wizardry; it’s the democratization of healthcare. It means that your chances of surviving a stroke may no longer depend on your zip code. A patient in a remote village in the Scottish Highlands could receive the same level of care, from the same world-class specialist, as someone in a major metropolitan hospital in London or New York.
This technology has the power to:
- Save Lives: By drastically reducing the time between diagnosis and treatment, it can significantly improve patient outcomes.
- Reduce Disability: Faster treatment means less brain damage, leading to better long-term recovery and quality of life.
- Bridge the Skills Gap: It allows the expertise of a few elite specialists to be scaled globally, serving a much larger patient population.
- Support Healthcare Systems: By treating patients locally, it reduces the immense cost and logistical burden of emergency patient transfers.
The development of robotic surgery systems like the Da Vinci has already shown how technology can augment a surgeon’s ability, offering greater precision and less invasive procedures (source). Remote thrombectomy is the logical, and revolutionary, next step in that journey.
AI Isn't Firing You… Yet. The Real Story Behind Tech's Layoff Storm
The Road Ahead: From Cadaver to Clinic
This successful test on a cadaver is a critical proof-of-concept. The next steps will involve rigorous testing, refinement, and eventually, in-human clinical trials. Engineers will work to further reduce latency, improve the tactile feedback for surgeons, and harden the system’s cybersecurity defenses. Medical bodies and governments will need to collaborate to create new legal and ethical frameworks for remote medical procedures.
While stroke care is a perfect first use-case due to its time-critical nature, the applications are endless. Imagine remote specialists performing emergency trauma surgery on a battlefield, conducting complex cancer operations for patients in developing nations, or even providing medical support for astronauts on a mission to Mars. The platform being built today is the foundation for a future where medical expertise is a globally available, on-demand resource.
The Cinema vs. Streaming Showdown: Why Your SaaS Startup Should Be Watching
Conclusion: The Future is Remote, Robotic, and Revolutionary
The Dundee-led remote thrombectomy is more than just a successful experiment; it’s a glimpse into the future of medicine. It represents a paradigm shift where physical distance is no longer a barrier to receiving the best possible care. This achievement stands on the shoulders of decades of progress in robotics, software engineering, cloud computing, and network infrastructure.
For the tech community, this is a call to action. The challenges of building this future—from writing perfectly reliable control software and creating predictive AI models to securing the network against all threats—are immense, but the reward is the chance to save millions of lives. The scalpel of the future may be held by a robot, but it will be guided by human ingenuity and powered by code.